
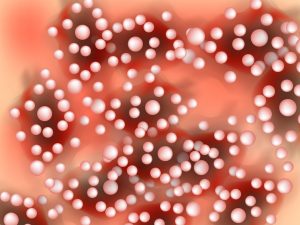
Pustular psoriasis is a rare and severe form of psoriasis characterized by white pustules (blisters of non-infectious pus) surrounded by red skin. This blog dives into the intricacies of pustular psoriasis, providing essential insights for those affected by this challenging condition and guidance on managing its symptoms effectively.
What is Pustular Psoriasis?
Pustular psoriasis is distinctly different from the more common plaque-type psoriasis. It is marked by the appearance of white pustules, which are filled with white blood cells called neutrophils. It can occur in isolated areas of the body, like the hands and feet (palmoplantar pustulosis), or can cover most of the body, which is known as generalized pustular psoriasis. This condition can be triggered by a variety of factors, including infections, stress, certain medications, or exposure to certain chemicals.
Symptoms and Diagnosis
The primary symptom of pustular psoriasis is the development of white pustules that can coalesce and scale over time. These pustules can be extremely painful and can lead to significant swelling. Additional symptoms may include fever, chills, severe itching, rapid pulse rate, fatigue, anemia, weight loss, and muscle weakness. Diagnosis typically involves a physical examination, detailed medical history, and sometimes a biopsy of the affected skin.
Management Strategies
Managing pustular psoriasis often requires a combination of systemic medications and topical treatments:
- Systemic treatments include medications that work throughout the body, such as biologics, which target specific parts of the immune system that drive inflammation; or systemic retinoids, which help to slow down the rate of skin cell growth and shedding.
- Topical treatments may involve corticosteroids, vitamin D analogs, or coal tar, which can help reduce inflammation and control flare-ups.
Lifestyle Adjustments and Home Care
Alongside medical treatments, making certain lifestyle adjustments can also significantly alleviate symptoms:
- Moisturizing regularly helps to keep the skin supple and reduces flaking and dryness.
- Avoiding known triggers such as stress, smoking, and alcohol can prevent or reduce flare-ups.
- Dietary changes, particularly incorporating anti-inflammatory foods and avoiding foods that can trigger inflammation, may also help manage symptoms.
Building a Support Network
Living with pustular psoriasis can be physically and emotionally challenging. It’s important for patients to build a strong support network that includes healthcare providers, family, friends, and possibly a mental health professional. Joining support groups, whether online or in person, can also provide emotional support and valuable information shared by others experiencing similar challenges.
Conclusion
While pustular psoriasis can be a demanding condition to manage, understanding its nature and having a comprehensive treatment plan can make a significant difference. Effective management relies on a combination of medical treatments, lifestyle adjustments, and strong support networks to help maintain quality of life and control symptoms. Remember, each person’s experience with pustular psoriasis is unique, and ongoing consultation with healthcare professionals is crucial to tailor treatments to individual needs.


